Sleep Apnea
Dr. Shannon treats sleep apnea and snoring with an oral appliance called a TAP appliance. Patients usually come in seeking an oral device after having tried, and not being able to tolerate a CPAP mask. Patients also will utilize an oral device as an adjunct to their CPAP machine. Many patients prefer to travel with a simple oral device rather than having to haul around a cumbersome CPAP machine through airport security. To be treated for sleep apnea with an oral device the patient must be diagnosed with sleep apnea from a medical physician and permission needs to be obtained from that physician to use an oral device. Permission is obtained by Dr. Shannon’s office and often times insurance will cover the cost of the oral device.
Patients will also utilize the TAP appliance for the elimination of snoring. Many times bed partners complain of snoring and can suffer from lack of sleep which can have medical implications if it becomes chronic. Snoring can also affect relationships as bed partners are often forced to sleep in different locations. Patients seeking an oral device to eliminate snoring do not need any diagnosis from a medical doctor nor would any permissions need to be obtained.
After reading below about sleep apnea please see photos at the bottom of the oral device (TAP Appliance) and the corresponding X-Rays.
Sleep apnea is a sleep disorder characterized by pauses in breathing or instances of shallow or infrequent breathing during sleep. Each pause in breathing, called an apnea, can last for several seconds to several minutes, and may occur, by definition, at least 5 times in an hour. Sleep apnea is a potentially serious sleep disorder and if left untreated can cause hypertension, stroke, or heart failure. You may have sleep apnea if you snore loudly, and you feel tired even after a full night’s sleep. The main types of sleep apnea are:
- Obstructive sleep apnea, the more common form that occurs when throat muscles relax.
- Central sleep apnea, which occurs when your brain doesn’t send proper signals to the muscles that control breathing.
- Complex sleep apnea syndrome, also known as treatment-emergent central sleep apnea, occurs when someone has both obstructive sleep apnea and central sleep apnea.
The signs and symptoms of obstructive and central sleep apneas overlap, sometimes making the type of sleep apnea more difficult to determine. The most common signs and symptoms of obstructive and central sleep apneas include:
- Loud snoring, which is usually more prominent in obstructive sleep apnea
- Episodes of breathing cessation during sleep witnessed by another person
- Abrupt awakenings accompanied by shortness of breath, which more likely indicates central sleep apnea
- Awakening with a dry mouth or sore throat
- Morning headache
- Difficulty staying asleep (insomnia)
- Excessive daytime sleepiness (hypersomnia)
- Attention problems
- Irritability
Obstructive sleep apnea occurs when the muscles in the back of your throat relax. These muscles support the soft palate, the triangular piece of tissue hanging from the soft palate (uvula), the tonsils, the side walls of the throat and the tongue. When the muscles relax, your airway narrows or closes as you breathe in, and you can’t get an adequate breath in. This may lower the level of oxygen in your blood. Your brain senses this inability to breathe and briefly rouses you from sleep so that you can reopen your airway. This awakening is usually so brief that you don’t remember it. You may make a snorting, choking or gasping sound. This pattern can repeat itself five to 30 times or more each hour, all night long. These disruptions impair your ability to reach the desired deep, restful phases of sleep, and you’ll probably feel sleepy during your waking hours. People with obstructive sleep apnea may not be aware that their sleep was interrupted. In fact, some people with this type of sleep apnea think they sleep well all night.
Central sleep apnea is a less common form of sleep apnea that occurs when your brain fails to transmit signals to your breathing muscles. This means you make no effort to breathe for a short period of time. You may awaken with shortness of breath or have a difficult time getting to sleep or staying asleep.
Sleep apnea is considered a serious medical condition. Complications may include:
- Daytime fatigue. The repeated awakenings associated with sleep apnea make normal, restorative sleep impossible. People with sleep apnea often experience severe daytime drowsiness, fatigue and irritability.
- You may have difficulty concentrating and find yourself falling asleep at work, while watching TV or even when driving. People with sleep apnea have an increased risk of motor vehicle and workplace accidents.
- You may also feel quick tempered, moody or depressed. Children and adolescents with sleep apnea may do poorly in school or have behavior problems.
- High blood pressure or heart problems. Sudden drops in blood oxygen levels that occur during sleep apnea increase blood pressure and strain the cardiovascular system. If you have obstructive sleep apnea, your risk of high blood pressure (hypertension) is greater than if you don’t.
- Obstructive sleep apnea may increase the risk of recurrent heart attack, and abnormal heartbeats, such as atrial fibrillation. Obstructive sleep apnea also increases the risk of stroke. If there’s underlying heart disease, these multiple episodes of low blood oxygen (hypoxia or hypoxemia) can lead to sudden death from an irregular heartbeat.
- Type 2 diabetes. People with sleep apnea are more likely to develop insulin resistance and type 2 diabetes compared with people without the sleep disorder.
- Metabolic syndrome. This disorder is a collection of other risk factors linked to a higher risk of heart disease. The conditions that make up metabolic syndrome include high blood pressure, abnormal cholesterol, high blood sugar and an increased waist circumference.
- Complications with medications and surgery. Obstructive sleep apnea is also a concern with certain medications and general anesthesia. People with sleep apnea may be more likely to experience complications following major surgery because they’re prone to breathing problems, especially when sedated and lying on their backs. Before you have surgery, tell your doctor that you have sleep apnea and how it’s treated.
- Liver problems. People with sleep apnea are more likely to have abnormal results on liver function tests, and their livers are more likely to show signs of scarring. This is a condition known as nonalcoholic fatty liver disease.
- Sleep-deprived partners. Loud snoring can keep those around you from getting good rest and eventually disrupt your relationships. It’s not uncommon for a partner to go to another room, or even on another floor of the house, to be able to sleep. Many bed partners of people who snore may be sleep-deprived as well.
Your doctor may make an evaluation based on your signs and symptoms or may refer you to a sleep disorder center. There, a sleep specialist can help you decide on your need for further evaluation. Such an evaluation often involves overnight monitoring of your breathing and other body functions during sleep. Home sleep testing may also be an option. Tests to detect sleep apnea may include:
- Nocturnal polysomnography. During this test, you’re hooked up to equipment that monitors your heart, lung and brain activity, breathing patterns, arm and leg movements, and blood oxygen levels while you sleep.
- Home sleep tests. In some cases, your doctor may provide you with simplified tests to be used at home to diagnose sleep apnea. These tests usually involve measuring your heart rate, blood oxygen level, airflow and breathing patterns. If you have sleep apnea, the test results will show drops in your oxygen level during apneas and subsequent rises with awakenings.
If the results are abnormal, your doctor may be able to prescribe a therapy without further testing. Portable monitoring devices don’t detect all cases of sleep apnea, so your doctor may still recommend polysomnography even if your initial results are normal. If you have obstructive sleep apnea, your doctor may refer you to an ear, nose and throat doctor to rule out any blockage in your nose or throat. An evaluation by a heart doctor (cardiologist) or a doctor who specializes in the nervous system (neurologist) may be necessary to look for causes of central sleep apnea.
For milder cases of sleep apnea, your doctor may recommend only lifestyle changes, such as losing weight or quitting smoking. And if you have nasal allergies, your doctor will recommend treatment for your allergies. If these measures don’t improve your signs and symptoms or if your apnea is moderate to severe, a number of other treatments are available. Certain devices can help open up a blocked airway. In other cases, surgery may be necessary. Treatments for obstructive sleep apnea may include:
- Continuous positive airway pressure (CPAP). If you have moderate to severe sleep apnea, you may benefit from a machine that delivers air pressure through a mask placed over your nose while you sleep. With CPAP (SEE-pap), the air pressure is somewhat greater than that of the surrounding air, and is just enough to keep your upper airway passages open, preventing apnea and snoring. Although CPAP is the most common and reliable method of treating sleep apnea, some people find it cumbersome or uncomfortable. Some people give up on CPAP, but with some practice, most people learn to adjust the tension of the straps to obtain a comfortable and secure fit. You may need to try more than one type of mask to find one that’s comfortable. Some people benefit from also using a humidifier along with their CPAP systems. Don’t just stop using the CPAP machine if you experience problems. Check with your doctor to see what modifications can be made to make you more comfortable. Additionally, contact your doctor if you are still snoring despite treatment or begin snoring again. If your weight changes, the pressure settings of the CPAP machine may need to be adjusted. Other airway pressure devices. If CPAP continues to be a problem for you, you may be able to use a different type of airway pressure device that automatically adjusts the pressure while you’re sleeping (Auto-CPAP). Units that supply bilevel positive airway pressure (BiPAP) are also available. These provide more pressure when you inhale and less when you exhale.
- Expiratory positive airway pressure (EPAP). These small, single-use devices are placed over each nostril before you go to sleep. The device is a valve that allows air to move freely in, but when you exhale, air must go through small holes in the valve. This increases pressure in the airway and keeps it open.The device may help reduce snoring and daytime sleepiness in people with mild obstructive sleep apnea. And it may be an option for some who can’t tolerate CPAP.
- Oral appliances. Another option is wearing an oral appliance designed to keep your throat open. CPAP is more reliably effective than oral appliances, but oral appliances may be easier to use. Some are designed to open your throat by bringing your jaw forward, which can sometimes relieve snoring and mild obstructive sleep apnea. A number of devices are available from your dentist. You may need to try different devices before finding one that works for you. Once you find the right fit, you’ll still need to follow up with your dentist repeatedly during the first year and then regularly after that to ensure that the fit is still good and to reassess your signs and symptoms.

TAP Appliance 
X-Ray with no oral device in place. Note the constriction of the airway behind the lower jaw.

TAP Appliance in the mouth 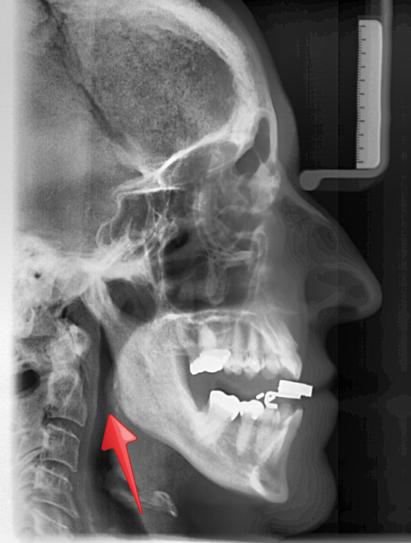
X-Ray with oral device in place. As you can see the device brings and holds the lower jaw forward therefore opening the airway. Note the dramatic difference in the space of the airway opening with versus without the oral device (TAP Appliance) in place.
